Bilateral Oophorectomy and Salpingectomy: Understanding the Procedures
Bilateral oophorectomy and salpingectomy are surgical procedures that involve the removal of the ovaries and fallopian tubes, respectively. These surgeries may be recommended for various medical reasons, including the treatment of gynecological conditions or as a preventative measure against certain health issues. In this detailed article, we will delve into the complexities of these procedures, their indications, and what patients can expect during recovery, highlighting the expertise available at DrSeckin.com.
1. What is Bilateral Oophorectomy?
A bilateral oophorectomy, also known as oophorectomy, involves the surgical removal of both ovaries. This procedure is often performed alongside a hysterectomy, where the uterus is also removed. The reasons for conducting a bilateral oophorectomy include:
- Ovarian Cancer: If there is a diagnosis of ovarian cancer or a family history suggesting a higher risk, doctors may recommend a bilateral oophorectomy.
- Endometriosis: Persistent and severe endometriosis that does not respond to other treatments may necessitate the removal of the ovaries.
- Genetic Risk Factors: Women with BRCA1 or BRCA2 gene mutations often choose to undergo bilateral oophorectomy as a preventive measure against breast and ovarian cancer.
- Benign Ovarian Tumors: Large, painful, or symptomatic benign tumors can necessitate their removal alongside the ovaries.
2. What is Salpingectomy?
Salpingectomy refers to the surgical removal of the fallopian tubes. This procedure can be performed alone or in conjunction with a bilateral oophorectomy. Salpingectomy is often indicated for:
- Ectopic Pregnancy: When a fertilized egg implants outside the uterus, it may require the removal of the affected fallopian tube.
- Preventive Measures: In some cases, salpingectomy is performed to reduce the risk of ovarian cancer, as emerging research suggests that some ovarian cancers may arise from the fallopian tubes.
- Infection: Severe infections or damage to the fallopian tubes may necessitate their removal to prevent further complications.
3. The Surgical Procedures
3.1 Preparing for the Surgery
Before undergoing either a bilateral oophorectomy or salpingectomy, patients will undergo a thorough evaluation that may include:
- Medical history assessment
- Physical examination
- Imaging tests (ultrasound, MRI, etc.)
- Blood tests to assess overall health
3.2 The Surgery Itself
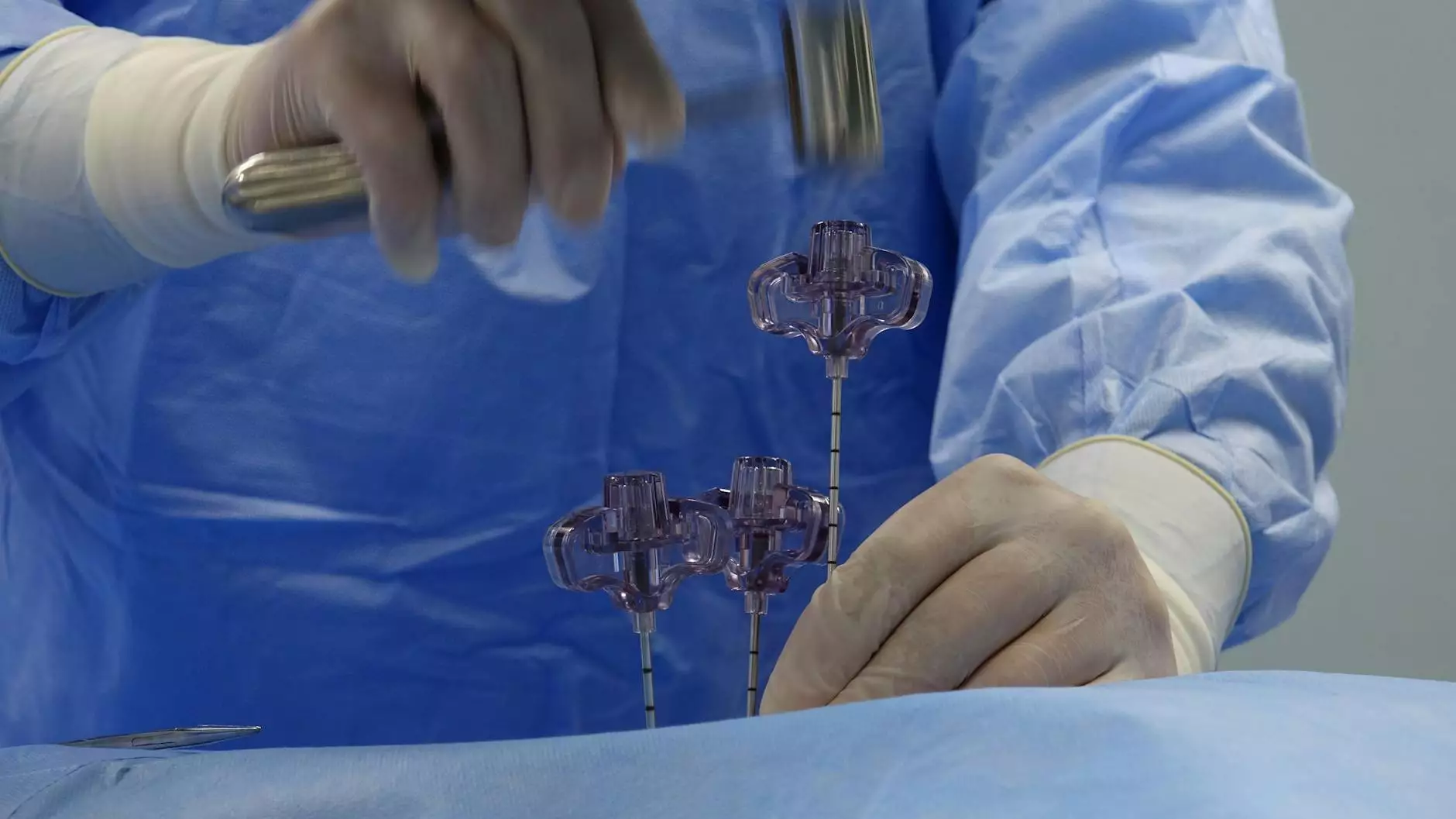
The surgical procedures can be performed using various techniques, including:
- Laparoscopic Surgery: This minimally invasive technique involves small incisions and the use of a camera to aid the surgeon. Patients often experience shorter recovery times with this method.
- Open Surgery: In some cases, traditional open surgery may be required, involving a larger incision to gain access to the reproductive organs.
The choice of technique will depend on factors such as the patient's specific medical condition, the extent of the surgery required, and the surgeon's expertise.
4. Recovery Process
Post-surgery recovery can vary by individual and surgical method. However, some common aspects of recovery include:
- Hospital Stay: Patients may stay in the hospital for observation, typically for one to two days following laparoscopic surgery and longer for open surgery.
- Pain Management: It’s normal to experience some discomfort. Doctors typically prescribe pain management strategies to ensure patient comfort.
- Activity Restrictions: Patients are generally advised to avoid heavy lifting and strenuous activities for several weeks post-surgery.
- Follow-Up Appointments: Follow-up care is paramount to monitor recovery and address any potential complications promptly.
5. Long-Term Implications
Undergoing a bilateral oophorectomy and salpingectomy has significant long-term implications that patients should consider:
- Hormonal Changes: The removal of the ovaries leads to a sudden drop in hormone levels, which can induce menopause. Patients will discuss with their healthcare provider about potential hormone replacement therapy (HRT).
- Fertility Considerations: These procedures are typically permanent forms of fertility control. Patients considering future pregnancy options should discuss alternatives with their healthcare provider.
- Psychological Impact: Patients may experience emotional changes after surgery. Support groups or counseling may be beneficial in navigating these feelings.
6. Choosing the Right Doctor
When contemplating surgical options, it is vital to choose a qualified and experienced surgeon. At DrSeckin.com, the team of expert obstetricians and gynecologists provide comprehensive care for women’s health, including thorough consultations and personalized surgical options tailored to individual needs.
6.1 What to Look For in a Surgeon
Here are key factors to consider when selecting a surgeon for bilateral oophorectomy and salpingectomy:
- Experience: Assessing the surgeon's experience with the specific procedures can provide confidence in their expertise.
- Patient Reviews: Researching reviews and testimonials from previous patients can offer insight into the surgeon’s skill and bedside manner.
- Communication: A surgeon should be able to effectively communicate the procedures, risks, and benefits clearly and patiently.
- Hospital Affiliations: The surgeon’s association with reputable hospitals can influence surgical outcomes and patient care.
7. Conclusion
In summary, bilateral oophorectomy and salpingectomy are significant surgical procedures with various implications for women’s health. Understanding the reasons, procedure, and recovery process can empower patients make informed decisions. The dedicated team at DrSeckin.com is here to provide expert guidance and care throughout your health journey, ensuring you receive the highest quality support tailored to your needs.









